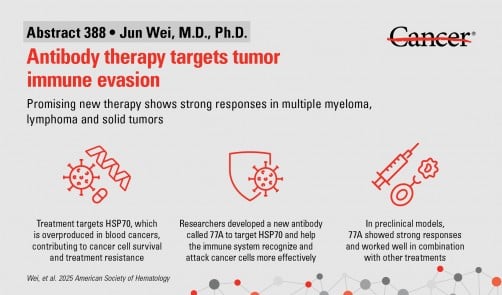
A groundbreaking therapy developed by researchers at The University of Texas MD Anderson Cancer Center shows promise in enhancing immune responses against blood cancers and solid tumors. The investigational antibody therapy, known as 77A, targets a cancer survival protein called HSP70, which helps tumors evade the immune system. Results were presented by Jun Wei, M.D., Ph.D., at the 67th American Society of Hematology (ASH) Annual Meeting in Orlando on December 6, 2025.
The study reveals that 77A can activate T cells and natural killer (NK) cells, ultimately reshaping the tumor environment to foster long-lasting immune responses. In laboratory models, the therapy significantly improved the effectiveness of chemotherapy, radiation, and other immunotherapies across various tumor types. Principal investigator Robert Z. Orlowski, M.D., Ph.D., emphasized the potential of this new approach, stating, “These results give us confidence that 77A could become a versatile immunotherapy.”
Mechanism of Action
The 77A antibody operates by specifically targeting HSP70, a heat shock protein frequently overproduced in certain blood cancers and solid tumors. This protein contributes to a hostile tumor microenvironment by suppressing immune responses and promoting cancer cell survival. In preclinical studies, 77A demonstrated strong antitumor effects by enhancing the activity of both innate and adaptive immune cells. It effectively improved the ability of immune cells to recognize and destroy cancer cells.
Additionally, 77A has shown promise when combined with existing treatments such as chemotherapy, radiation therapy, and immune checkpoint inhibitors. It also holds potential for integration with adoptive T cell therapy, a modern technique that utilizes lab-grown immune cells to target cancer cells.
Future Directions
Early tests involving human immune cells have indicated that 77A could enhance immune responses in healthy donors. These encouraging findings point towards the possibility of clinical trials, setting the stage for 77A to emerge as a versatile therapeutic option. Orlowski remarked, “Our next step is to advance a humanized version of this antibody into clinical trials to evaluate its potential in patients across multiple cancer types.”
The development of the 77A humanized antibody is currently underway, with expectations to initiate clinical trials soon. This study received support from Blood Cancer United, formerly known as the Leukemia & Lymphoma Society. A complete list of collaborating authors and their disclosures is available with the abstract.
As researchers continue to explore the therapeutic potential of 77A, the medical community remains optimistic about the advancements in immunotherapy and its ability to transform cancer treatment landscapes.