Cardiovascular disease (CVD) remains the leading cause of death across various communities, but certain groups, including low-income individuals, women, racial minorities, and rural residents, face disproportionately higher rates of heart attacks, strokes, and limb loss. Dr. Lee Kirksey, a Cleveland vascular surgeon and health equity advocate, emphasizes the urgent need to address the concept of “cardiovascular deserts,” regions lacking adequate access to cardiologists, primary care physicians, and hospitals.
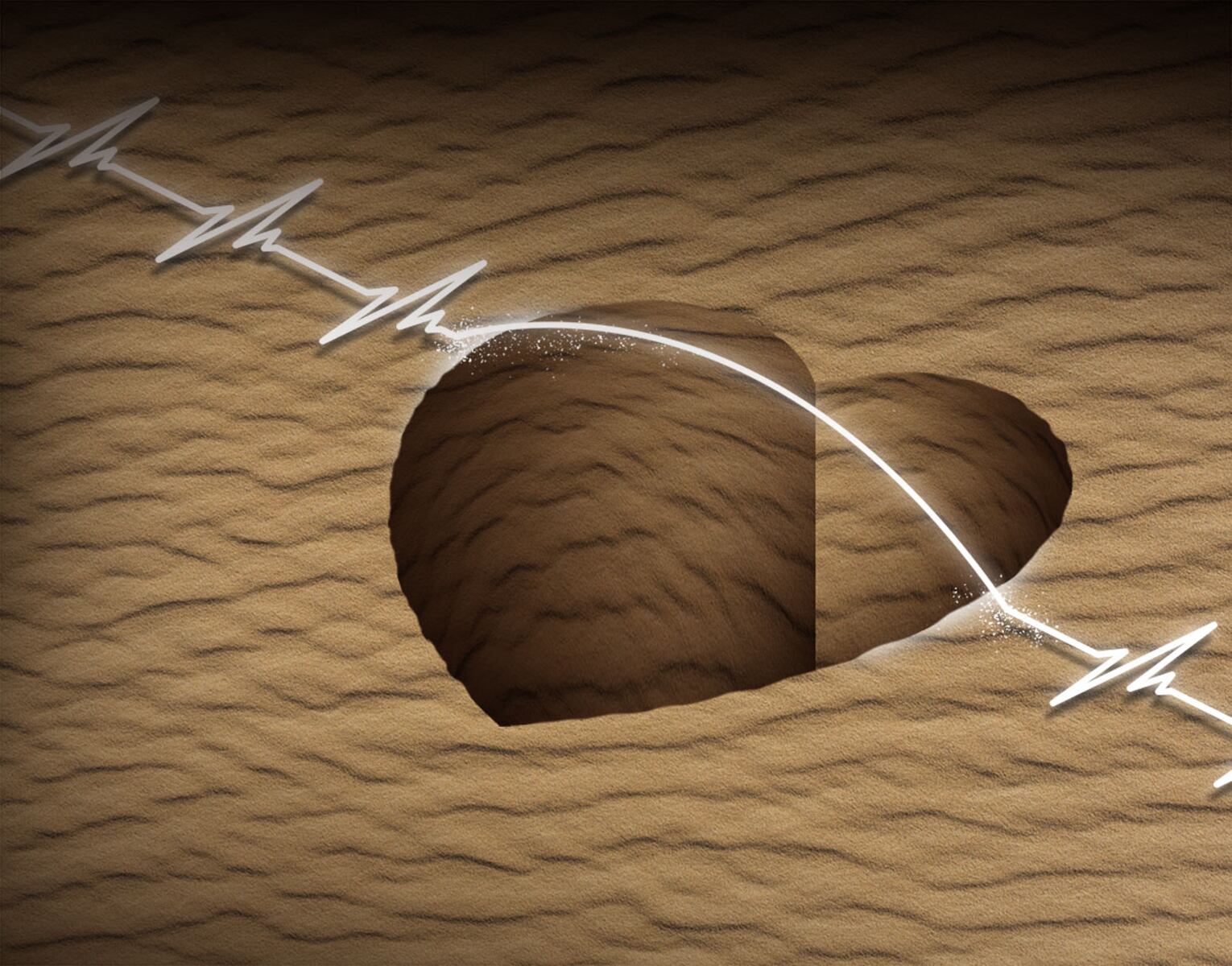
The term “cardiovascular desert” highlights the geographic disparity in healthcare access. Factors such as obesity, diabetes, high cholesterol, and smoking contribute to CVD prevalence, exacerbated by systemic barriers like low health insurance coverage. Dr. Kirksey’s background in the rural community of Alliance, Ohio, illustrates the challenges faced by those living far from major medical facilities. For residents, what appears as a short distance on a map often translates into long travel times, missed workdays, and lost income.
Life expectancy gaps between rural and urban communities have widened since the 1990s, correlating with economic downturns, particularly in regions that once thrived on manufacturing. The decline of industries such as steel and automobiles has left a lasting impact on these areas. Dr. Kirksey highlights that while physical distance is a significant factor in healthcare disparities, other underlying issues, including political will and socioeconomic drivers, create “deserts” even within metropolitan areas.
Recent legislation, particularly the One Big Beautiful Bill Act (OBBBA), signed into law on July 4, 2025, raises concerns regarding its implications for vulnerable communities. The act is set to reduce federal Medicaid spending by over $900 billion over the next decade. The American Medical Association predicts that this will lead to more than 11 million people potentially losing their coverage due to new administrative requirements and work mandates.
The OBBBA also eliminated the Grad Plus Loan program, which previously allowed medical students to borrow funds for tuition and living expenses. This change is expected to deter applications from lower-income students, worsening the existing physician shortages in underserved areas. Research indicates that individuals from low-income and rural backgrounds are more likely to return to their communities to practice medicine, underscoring the need for systemic support.
On the treatment front, medications such as Wegovy and Ozempic have transformed the management of diabetes and obesity, which in turn reduces cardiovascular events. Yet, access to these medications remains inconsistent across public and private insurance plans, with out-of-pocket costs reaching as high as $1,000 per month for some patients. This situation exacerbates the disparity between those who can afford these innovations and those who cannot.
Telehealth presents a potential solution to bridge the gap in access to care in cardiovascular deserts. However, significant challenges must be addressed. Partnerships with broadband providers are essential to enhance community connectivity and expand affordable internet access. The “Digital Divide” remains a critical issue, particularly in vulnerable communities where digital literacy is low. Educating patients on the use of remote health technology is crucial for successful telehealth implementation.
Furthermore, long-term commitment to telehealth reimbursement by payers is necessary to incentivize investment in healthcare infrastructure. Developing best practices and ensuring consistent provider participation will be vital in leveraging telehealth to improve care access.
Dr. Kirksey concludes with a strong message, emphasizing the importance of remembering communities that represent the best of Ohio. The existence of cardiovascular deserts highlights the broader dimensions of health disparities that require dedicated political action, collaborative partnerships, and tailored strategies for effective resolution. Addressing these disparities is not just a healthcare issue; it is a matter of social justice and equity in health access.