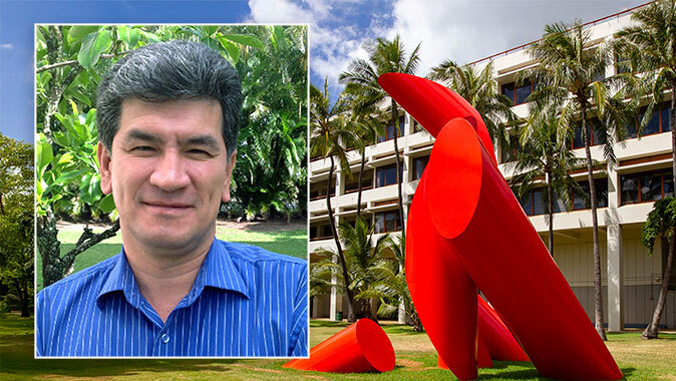
The management of non-small cell lung cancer (NSCLC) is experiencing a significant shift with the introduction of new biomarker testing methods. This evolution extends beyond traditional genomic analysis to include protein-based and computationally derived markers. These advancements are largely driven by the approval of innovative therapies, particularly antibody-drug conjugates (ADCs), and an enhanced understanding of therapeutic resistance, as outlined by Dr. Soo-Ryum Yang, during his presentation at the 20th Annual New York Lung Cancers Symposium on November 15, 2025.
Dr. Yang, who serves as an assistant attending pathologist and co-director of Clinical Biomarker Development at Memorial Sloan Kettering Cancer Center in New York, emphasized four key trends shaping the future of NSCLC treatment. These include the rise of protein-based immunohistochemistry (IHC) biomarkers for ADCs, the actionable nature of tumor suppressor genes, the potential of synthetic lethality in therapy, and the integration of computational pathology.
A critical challenge remains the scarcity of tissue samples, which necessitates the development and implementation of multiplex IHC techniques. This approach, paired with broad panel next-generation sequencing (NGS) and artificial intelligence (AI), aims to expand personalized therapy options for a larger segment of the NSCLC patient population. Dr. Yang pointed out that the focus has shifted from solely identifying mutated genes to measuring protein expression levels, which can reveal new treatment avenues.
Established IHC testing for PD-L1 has guided checkpoint inhibitor therapy, but it is now also being adapted for guiding ADC usage. Two essential protein biomarkers in NSCLC highlighted by Dr. Yang are HER2 and c-MET overexpression. HER2 overexpression occurs in as many as 20% of patients, with the highest expression levels (IHC 3+) found in up to 3%. Notably, Dr. Yang explained that there is no direct correlation between HER2 mutation status and overexpression, which complicates treatment decisions.
The approval of fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu) for HER2-positive solid tumors, including NSCLC patients who have undergone previous treatments, was supported by the phase 2 DESTINY-Lung01 study. Dr. Yang advocated for the application of gastric cancer HER2 scoring guidelines to NSCLC testing. Similarly, actionable c-MET-high status, defined as over 50% of tumor cells exhibiting 3+ staining, is observed in up to 17% of cases with wild-type EGFR.
In May 2025, the FDA granted accelerated approval to telisotuzumab vedotin (teliso-V; Emrelis) for this patient demographic, following evidence from the phase 2 LUMINOSITY trial. Dr. Yang proposed that the integration of HER2 and c-MET IHC screening presents substantial challenges for current diagnostic workflows. He suggested a flexible strategy that allows institutions to optimize their testing processes according to available resources and expertise.
Numerous biomarkers are under investigation, with potential to refine personalized treatment for NSCLC patients. For instance, KRAS mutations are prevalent in approximately 40% of lung adenocarcinomas, particularly in codons G12, G13, and Q61. Notably, the KRAS G12D mutation is linked to a history of minimal or no smoking and results in a lower tumor mutational burden, complicating treatment outcomes. Established therapies such as sotorasib (Lumakras) and adagrasib (Krazati) target KRAS G12C mutations, while ongoing clinical trials explore therapies aimed at additional KRAS mutations.
Dr. Yang also noted the significance of STK11 and KEAP1 mutations, which occur in up to 20% of lung cancers and often co-exist with KRAS mutations. These mutations foster an immunosuppressive tumor microenvironment, leading to resistance to immunotherapy. Recent findings from the phase 3 POSEIDON trial indicate that combining a CTLA-4 inhibitor with a PD-L1 inhibitor and chemotherapy can enhance outcomes for such patients.
Emerging therapeutic targets like MTAP deletions in cancer cells present additional opportunities for treatment innovation. Dr. Yang explained that targeting the enzyme PRMT5, which is impaired by MTAP deletions, can induce selective cancer cell death through a synthetic lethality approach. MTAP deletions are found in up to 18% of lung cancers and are associated with poor responses to immunotherapy.
As the landscape of NSCLC treatment evolves, the introduction of TROP2 as a target for ADC development highlights ongoing advancements. The anti-TROP2 ADC, datopotamab deruxtecan-dlnk (Dato-DXd; Datroway), is currently being evaluated as a second-line therapy. While the phase 3 TROPION-Lung01 study demonstrated a progression-free survival benefit, it did not show a statistically significant overall survival advantage.
To enhance predictive capabilities, researchers have developed an AI-driven approach that quantitatively assesses TROP2 staining, potentially improving treatment response assessments. Although promising, Dr. Yang cautioned that this approach requires further validation and raises questions about accessibility across various digital pathology platforms.
The ongoing advancements in biomarker testing signify a broader and more holistic approach to NSCLC management, moving beyond a singular focus on genomics. As Dr. Yang noted, the future of lung cancer treatment lies in the integration of protein analysis, AI insights, and innovative therapeutic strategies, making personalized medicine an achievable goal for a wider patient population. He concluded that comprehensive biomarker testing will increasingly rely on multiplex IHC and NGS in the coming years, paving the way for enhanced treatment options.